About Atrial Fibrillation
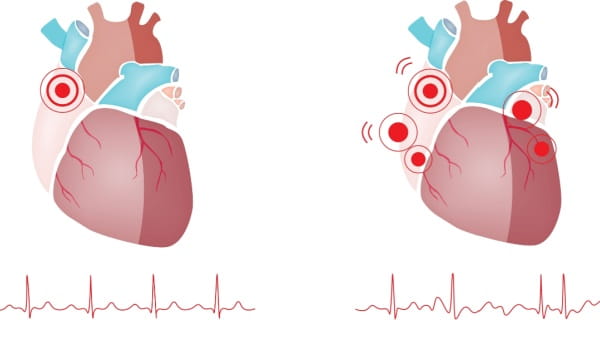
Atrial fibrillation (AFib) is an arrhythmia (heart rhythm disorder) causing a rapid, irregular heartbeat that disrupts blood flow. In a healthy heart, the heart's two upper chambers, called the atria, beat in sequence with the two lower chambers, called the right and left ventricles. In a patient with AFib, the atria beat faster than and out of sync with the ventricles. The result is a very rapid and disorganized heartbeat. According to the Centers for Disease Control and Prevention, an estimated 6.1 million people in the U.S. suffer from atrial fibrillation.
Types of AFib
-
Paroxysmal AFib
-
Persistent AFib
-
Permanent AFib
-
Postoperative AFib
-
Valvular AFib
- Heart Palpitations – a sudden feeling that your heart is racing, pounding, or fluttering
- Lack of energy or feeling overtired
- Dizziness or feeling lightheaded
- Fainting
- Weakness
- Shortness of breath or trouble breathing
- Confusion
- Chest pain or discomfort
If you're experiencing pressure, heaviness or pain in the chest, arm or below the breastbone alone or in combination with sweating, nausea, extreme shortness of breath or irregular heartbeats, you may be having a heart attack. Call 911 immediately.
Causes and Risk Factors
Some people are born with abnormalities that cause AFib, while others develop the condition due to related medical conditions, such as high blood pressure, heart attacks, overactive thyroid glands, emphysema, sleep apnea, or previous heart surgeries. AFib may begin as a less serious heart arrhythmia called atrial flutter. Most of the time, there is no underlying heart disease causing AFib. However, there are risk factors that could increase your chances of developing the condition:- Having pre-existing conditions
- Existing heart conditions, such as high blood pressure (hypertension), coronary artery disease, or heart valve disease
- Chronic lung disease
- Chronic medical conditions such as overactive thyroid and diabetes
- Excessive consumption of alcohol or caffeine
- Taking certain medications
- Stress
- Smoking tobacco
- Being male and 55 years of age or older
If you have a family history of heart conditions or one or more of the risk factors for AFib, talk to your primary care doctor about preventive care.
Need a primary care physician? Select family or internal medicine on our form below.
Diagnosing AFib
To determine if someone has AFib, various diagnostic tests are essential. These tests help doctors diagnose and recommend personalized treatment. Diagnosing AFib usually begins with a cardiologist performing a comprehensive physical exam and discussing symptoms and medical history. Your cardiologist may refer you to an electrophysiologist for advanced testing and treatments. Diagnostic procedures include:
- Blood tests
- Chest X-ray
- Echocardiogram (echo): an ultrasound of your heart
- Holter monitor test, which monitors your heart's activity over a period of time
- Electrocardiogram (ECG): a measure of your heart's electrical activity
- Electrophysiologic testing (EP studies): these procedures are performed in our sophisticated electrophysiology (EP) labs, equipped with high-resolution imaging technology and heart mapping systems
Already have an order from your doctor for blood tests or imaging? We have you covered!
Schedule at one of the many BayCare locations.
Treatment Options
With proper care and treatment, AFib can be controlled, and most people lead normal lives. Left untreated, AFib can lead to a high risk of stroke, heart failure and sudden cardiac arrest. The treatment of AFib has three goals: (1) control of symptoms, (2) stroke prevention and (3) treatment of the underlying risk factors. Treatment can:- Increase quality of life
- Decrease risk of stroke
- Decrease symptoms of AFib
- Decrease use of medication
-
Lifestyle Changes
-
Medications
-
Cardioversion
-
Ablation Procedures
-
Cox Maze Surgery
Various types of medications are used to help control the rate at which your heart pumps as well as restore the heart’s normal beating rhythm.
- Beta or calcium channel blockers - Drugs to help control your heart’s rate that slow down how fast the heart pumps in different ways.
- Sodium or potassium channel blockers - Drugs to help control your heart’s rhythm by slowing the conduction of electrical signs through the muscle.
These are procedures where our heart rhythm specialists (electrophysiologists) use advanced technology to treat the heart tissue causing irregular heartbeat. Treatment creates small amounts of scar tissue that blocks the abnormal electrical impulses causing AFib and restores the heart's normal rhythm. We offer several different types of ablation procedures including minimally-invasive hybrid convergent ablation. The following locations offer this procedure:
- Morton Plant Hospital in Clearwater
- St. Joseph's Hospital in Tampa
- Winter Haven Hospital in Winter Haven
During this complex procedure, your surgeon stops the abnormal electrical impulses using a complicated "maze" of incisions on the atria (upper chambers) of the heart. You may be a candidate for the Cox Maze procedure if you have permanent AFib, enlarged atria (the upper chambers of the heart), or if you have had a previous failed catheter ablation procedure. The following locations offer this procedure:
- Morton Plant Hospital in Clearwater
- St. Joseph's Hospital in Tampa
- Winter Haven Hospital in Winter Haven
AFib and Stroke Risk
According to the American Heart Association, someone with AFib is five times more likely to have a stroke compared to those without it. In fact, 15 percent of all strokes occur in people with AFib. When the atria are beating rapidly and irregularly, it may cause blood to pool in the heart. This may lead to blood clots, which can travel to the brain and cause a stroke. In people with AFib not caused by heart valve problems, most the of stroke-causing clots that come from the heart are form in a small pouch called the left atrial appendage (LAA) connected to the heart.
In addition to medications, there are devices that can reduce the risk of stroke. These devices may be appropriate for patients who cannot take medications due to certain risk factors. There are two categories of devices:
-
Epicardial
-
Endocardial
Epicardial devices are devices placed outside of the heart. During these procedures, a device or stitch is placed around the LAA, closing it and blocking blood clots from forming there and traveling to the brain. Common devices include the LARIAT and AtriClip. The following locations offer these procedures:
- Morton Plant Hospital in Clearwater
- St. Joseph's Hospital in Tampa
- Winter Haven Hospital in Winter Haven
Endocardial devices are placed inside of the heart. During these procedures, a device is implanted inside the LAA using a catheter. The device acts as a permanent barrier to prevent blood clots from forming there and is only recommended for patients whose AFib is not caused by heart valve problems. Common devices include the WATCHMAN and Amulet Amplatzer. The following locations offer these procedures:
- Morton Plant Hospital in Clearwater
- St. Joseph's Hospital in Tampa
- Winter Haven Hospital in Winter Haven
Living With AFib
Many people can live a long and normal life with AFib. It is important to be diagnosed, treated and monitored by a cardiologist. While AFib isn’t typically curable, you can reduce symptoms and risk factors with proper care. Alongside medical recommendations, certain lifestyle changes including diet and exercise may be helpful too. These will help to lower your risk factors for developing other conditions such as heart disease, heart failure and stroke.
Before making any changes, always consult your doctor to make sure you understand how to prevent any potential complications from AFib. When researching AFib and treatment options, use reliable sources such as the National Institutes of Health and others your physician recommends.
Additional Resources
Frequently Asked Questions
-
If I think I may have AFib, where do I start?If you suspect you have AFib symptoms such as heart racing, shortness of breath, chest pain, weakness and more, please make an appointment with one of our BayCare heart specialists. General cardiologists or electrophysiologists can diagnose AFib. Even if your symptoms go away, it is important to consult a doctor. If you need a heart doctor, please fill out our referral form or call (855) 233-0888. If you are having a medical emergency, please call 911 immediately.
-
Is AFib curable?AFib is not typically curable, but symptoms can be managed or controlled and risk factors can be decreased with proper care and management by a heart specialist.
-
Why is AFib dangerous?AFib is a serious and dangerous condition because it affects the heart’s ability to fill with blood as it should. Blood clots may form. This increases the risk for stroke. Untreated, it can also lead to heart disease and heart failure. AFib can be controlled. With treatment, most people lead normal lives.
-
Can I live a long life with AFib?Yes, most people with AFib can live a long and normal life with proper medical care and symptom control.
-
If I am having an AFib episode, what should I do?If you are in great discomfort and your heart is beating very rapidly and irregularly, please call 911 or get to the nearest emergency room. Staff in an emergency room can determine the most appropriate way to get your heart back to normal rhythm. Unlike a heart attack, most episodes of AFib are usually not life threatening. After an ER visit, it is important to follow-up with a heart specialist like your cardiologist or electrophysiologist. Need a cardiologist or electrophysiologist specialist? Call us at (855) 233-0888 for a physician referral or fill out the form to request a referral to a cardiac specialist that meets your needs.
-
What questions should I ask my doctor about AFib?
Thinking about and writing down a list of questions to ask your heart specialist about AFib is a great way to get the most out of an appointment with a cardiologist or electrophysiologist. To help you prepare, here is a list of questions you may want to ask your physician. We want to empower and educate you to make the most informed decisions about care for your heart. Example of questions to ask your doctor:
- What could be the cause of my AFib?
- How can I be sure I have AFib and not a more serious heart rhythm or other heart problem?
- What are the risks that my AFib will become worse (more symptomatic)?
- What risk factors should I be most concerned about?
- What medications may be recommended to treat my AFib?
- What procedures might be best for me? What are the risks, benefits and success rates of each?
- What is the long-term effect of AFib on my heart?
- Can I exercise safely?
- What should I do if I forget a dose of my medication?
Find a Location
With more than 25 years of highly specialized clinical expertise in treating heart rhythm disorders like AFib, BayCare’s teams’ of heart specialists use the latest in advanced electrophysiology technology to map heart rhythm disorders and provide innovative treatments. Learn more about our outstanding facilities that provide treatment for AFib.
Need a cardiac electrophysiologist or other cardiac specialist?
Call us at (855) 233-0888 or fill out the form to request a referral to a cardiac specialist.